7667766266
enquiry@shankarias.in
Why in news?
WHO has allowed widespread use of the world’s first malaria vaccine, RTS,S as part of a pilot project in parts of Africa.
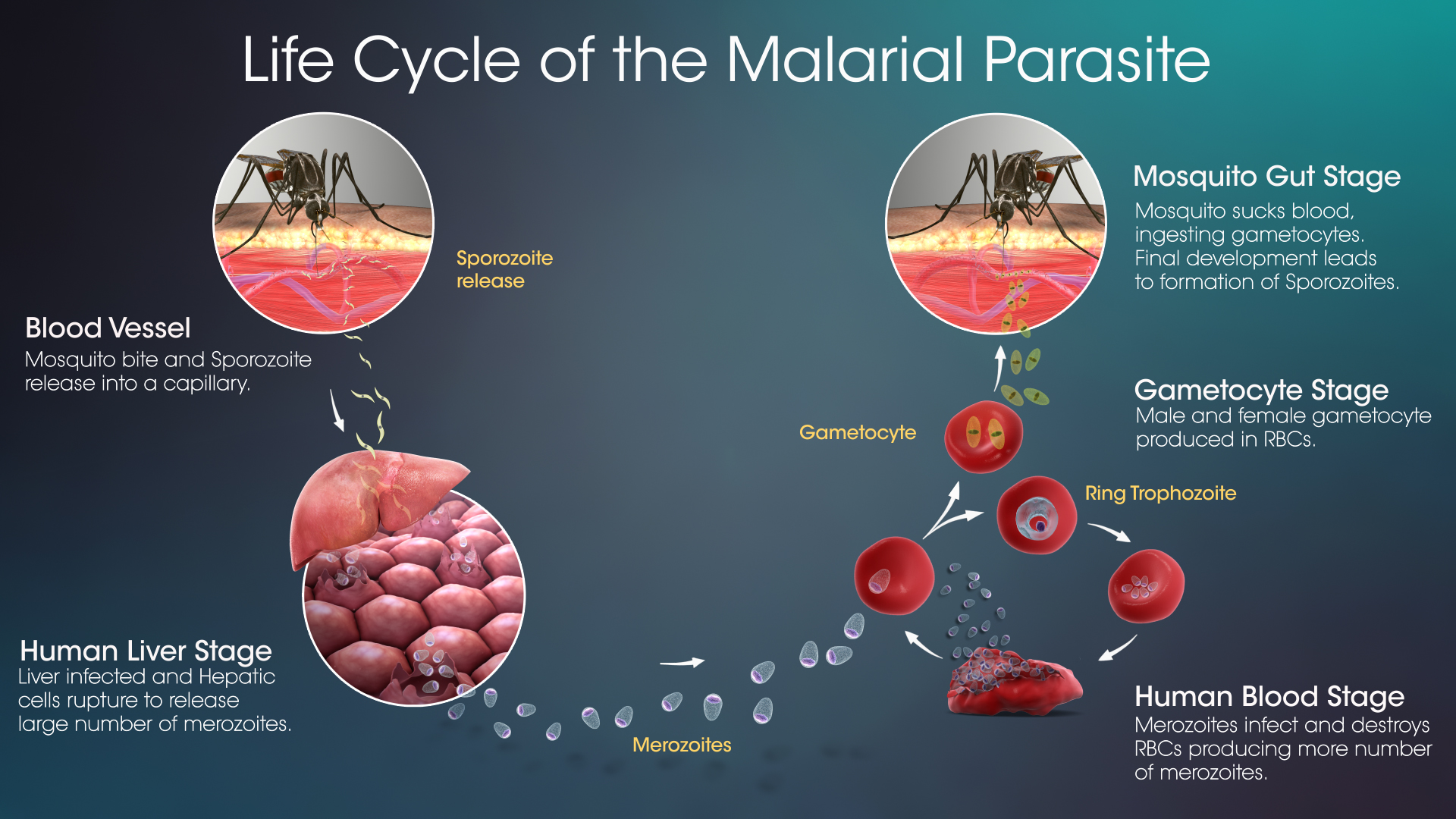
What is Malaria?
What is the status of Malaria?
What is the vaccine that has been cleared for widespread use?
What measures have been taken to eliminate malaria?
Over the last two decades, 11 countries have been certified by the WHO Director-General as malaria-free - UAE, Morocco, Turkmenistan, Armenia, Sri Lanka, Kyrgyzstan, Paraguay, Uzbekistan, Algeria , Argentina and El Salvador
What are the challenges in the elimination of Malaria?
What measures needs to be taken?
Source: The Indian Express, The Hindu