7667766266
enquiry@shankarias.in
Mains: GS II – Issues Relating to Development and Management of Social Sector/Services relating to Health, Education, Human Resources.
Recently there has been a considerable improvement in the mental health of people due to various efforts taken by the government of India.
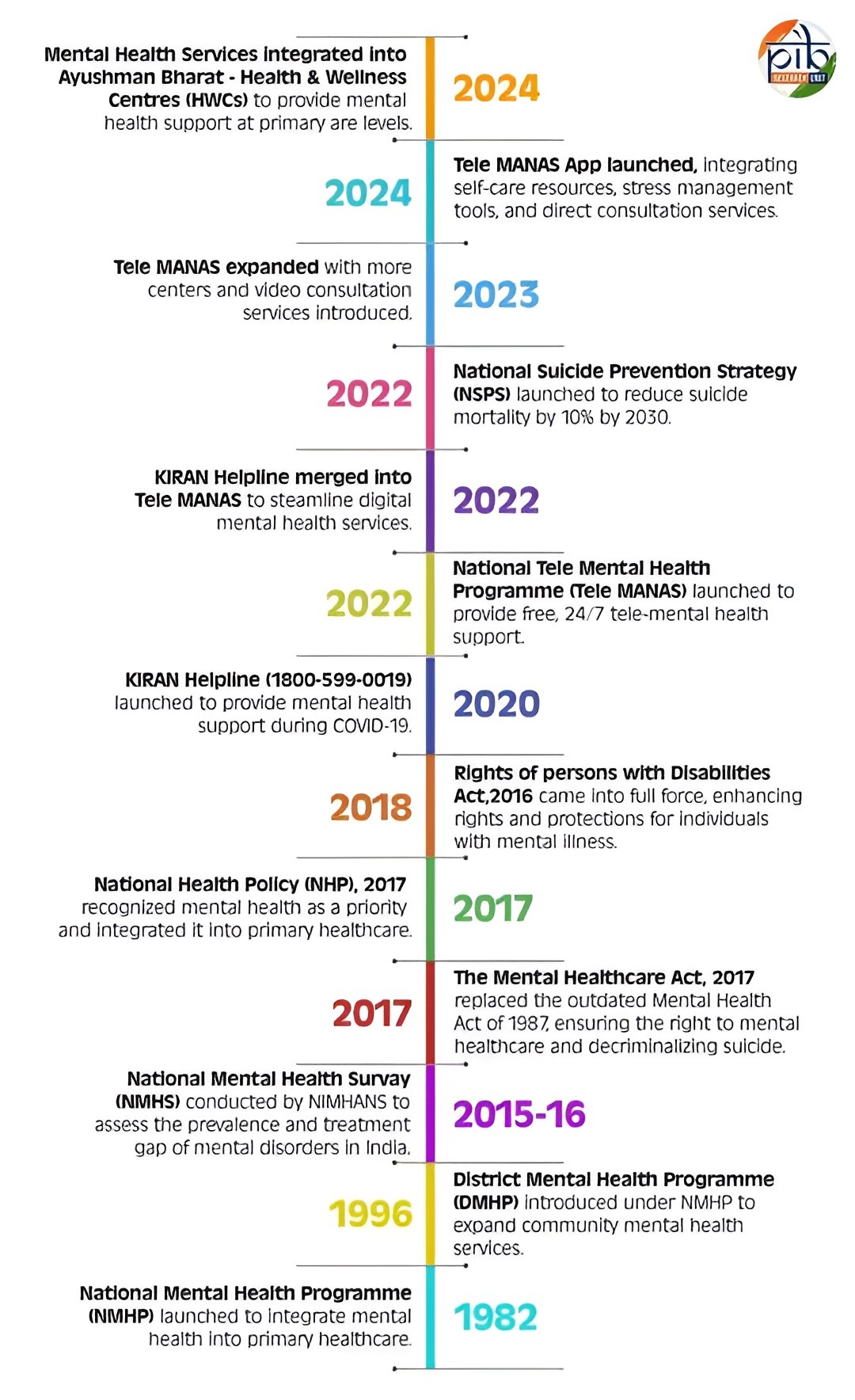
The World Health Organization (WHO) praised Tele MANAS as an effective and scalable mental health solution, making mental healthcare more inclusive and affordable.

Ministry of Health and Family Welfare| Mental Health